Author: Marcy Burnham, RN, AED365 Leader
Cardiac arrest occurs when the heart suddenly stops beating, preventing blood flow to the brain and other vital organs. Immediate response is critical, as survival rates decrease by about 10% with each minute that passes without intervention. Unfortunately, the likelihood of survival can vary drastically depending on where a cardiac arrest occurs and who and what resources are nearby. We need to work towards closing the cardiac arrest survival gap and ensuring that every individual has an equal chance of survival in the face of this critical medical emergency. Some strategies to consider in helping to close the survival gap include prioritizing public awareness, expanding access to life-saving tools, and addressing systemic inequalities.
Public knowledge about cardiac arrest and the importance of immediate intervention, such as performing CPR and using AEDs, varies widely. Communities with limited access to educational resources and training programs often see lower bystander intervention rates. Increasing public awareness about cardiac arrest and the importance of early intervention is crucial. Community-based programs should focus on CPR and AED Training and public awareness campaigns.
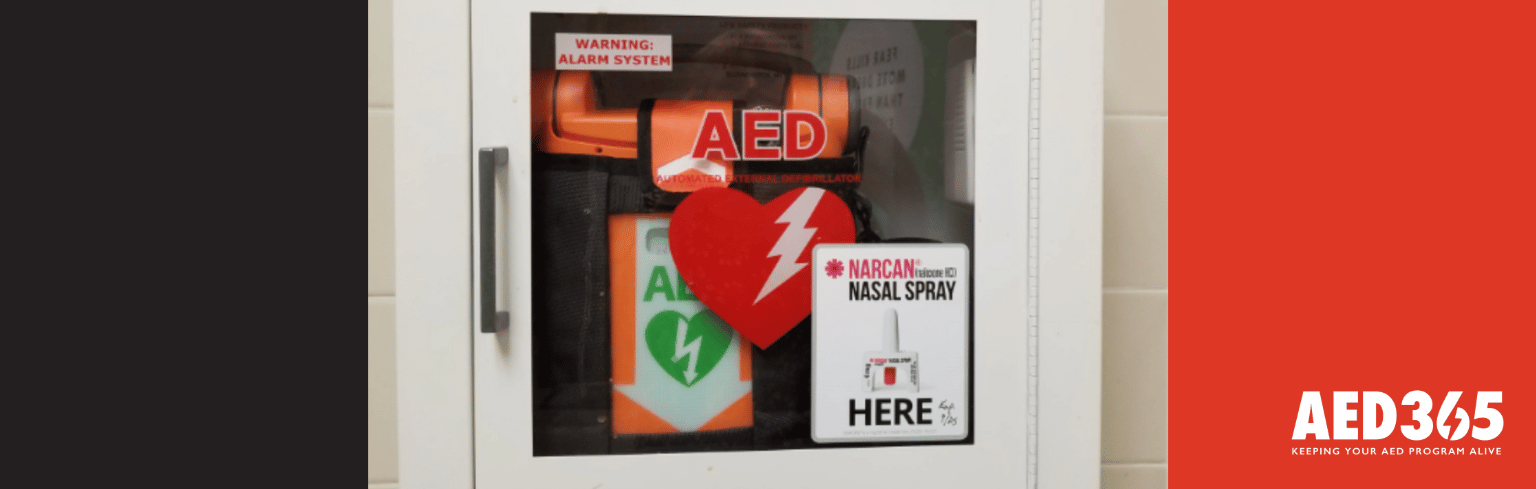
Sharing and expanding lifesaving knowledge is essential in closing the survival gap, and even more effective when coupled with proper, accessible equipment. Ensuring AEDs are available in high-traffic areas such as airports, malls, and sports venues is critical. Also, implementing policies that support the placement of AEDs in rural and underserved communities can reduce response times and improve outcomes. Partnerships with businesses and community organizations can facilitate this expansion into rural areas, as well.
Expanding access to preventive healthcare services in underserved communities can help reduce the incidence of cardiac arrest by managing risk factors such as hypertension and diabetes. Community engagement and collaborating with local leaders and organizations to identify barriers and develop tailored solutions for specific communities will contribute tremendously.
Working together and educating ourselves on the needs of different communities are essential in shrinking the SCA survival gap. It is important to consider these suggestions when developing a strategy for sharing lifesaving skills, equipment, and knowledge with others. Let’s make sure we do our part in bridging this gap and increasing SCA survival rates across the globe.
Office: (205) 417-4711
Email: info@aed365.com